Traumatic brain injury can occur when a sudden, brutal blow or jolt to the head causes brain damage. This is a major cause of illness and death in the United States, and elsewhere.
When the brain collides with the skull ‘s interior, the brain can be swollen, the nerve fibers teared, and bleeding. When the skull fractures, the brain tissue may be penetrated by a broken piece of skull.
Causes include falls, injuries to sports, gunshot wounds, physical assault and road traffic accidents.
The Centers for Disease Control and Prevention ( CDC) defines a TBI as “a disruption in normal brain function that may be caused by a bump, blow, or jolt to the head, or penetration of head injury.”
The severity of symptoms will depend on the part of the brain is affected, whether it is at a particular location or over a large region, and the extent of the damage.
The transient discomfort and headache can occur in mild cases. Severe TBI can lead to unconsciousness, amnesia, paralysis, coma and long-term illness or death.
The CDC reports TBI was leading to the deaths of about 50,000 people in 2013. In 2012, 329,290 people under the age of 19 applied for emergency care for a TBI arising from a sporting or recreational activity.
Parents , guardians and teachers will ensure that children are adequately monitored during sports and other events and that they wear acceptable safety equipment.
A head injury or suspected TBI needs medical attention.
Important facts about traumatic brain injury
- The effect of a TBI, such as concussion, depends on the severity of the injury and where it occurs.
- It is a major cause of death and disability in the United States and worldwide.
- Causes include falls, road traffic accidents, and sports injuries.
- Symptoms include confusion, persistent headaches, convulsions, and memory loss.
- Anyone who receives a head injury, however mild, should consider seeking medical attention.
Symptoms

Signs and symptoms may appear immediately, within 24 hours, or may develop days or weeks after the injury. Symptoms are sometimes subtle. A person may notice an issue but does not relate it to the injury. After a TBI, some people will appear to have no symptoms but their condition later worsens.
The effects can be both psychological and physical.
The initial physical effects include swelling and bruising. Increased brain pressure can cause:
- damage to brain tissue, as it presses against the skull or as one part of the brain pushes into another
- pressure on blood vessels, reducing their ability to supply the brain cells with oxygen and essential nutrients
Internal bleeding
Signs of internal bleeding include bruise behind the ears (sign of battle) or around the body (body of raccoon). This can actually result in a serious or life-threatening injury. They require urgent medical treatment.
Other signs that may indicate severe injury include:
- a loss of consciousness
- convulsions or seizures
- repeated vomiting
- slurred speech
- weakness or numbness in the arms, legs, hands, or feet
- agitation
- loss of coordination
- dilated pupils
- inability to wake up from sleep
- severe headache
- weakness and numbness in hands, feet, arms or legs
The following signs and symptoms can also indicate a need for urgent attention:
- confusion
- changes in mood
- memory problems
- inability to remember what happened before or after the incident
- fatigue (tiredness) and lethargy
- getting lost easily
- persistent headaches
- persistent pain in the neck
- slowness in thinking, speaking, reading or acting
- moodiness, for example, suddenly feeling sad or angry for no apparent reason
- sleep pattern changes, such as sleeping more or less than usual, or having trouble sleeping
- light headedness, dizziness
- becoming more easily distracted
- increased sensitivity to light or sounds
- loss of sense of smell or taste
- nausea
- tinnitus, or ringing in the ears
Those can come up at once, in hours, or later. A person who has sustained a TBI but does not appear to have any symptoms should be closely watched for 24 hours, because there might not be obvious signs of injury.
Someone who suffers from the aforementioned symptoms even days or weeks after a TBI should see a physician.

Children may have the same signs and symptoms but will have less chance of letting others know how they feel.
When an infant has had a hit or jolt to the head and there are any of the following signs or symptoms, call a doctor.
- changes in sleeping patterns
- irritability and crying
- listlessness
- loss of balance
- loss of newly acquired skills, such as toilet training
- changes in playing behavior changes
- refusal to eat
- loss of interest in favorite activities or toys
- tiredness
- unsteady walking
- vomiting
If these signs are noticed, the child should see a doctor.
In sport, the game should be left out by the player and not play again until the doctor gives permission to enter, whether or not they lose consciousness. Not all TBI or concussion causes a loss of consciousness.
In the long run repeated head injuries can be especially damaging to the brain in rapid succession.
An individual who has had a TBI should be monitored as their condition can deteriorate rapidly and symptoms that seem mild can get serious.
Long-term effects
There is that evidence that a TBI or repeated TBIs may have long-term health consequences including increased risk of dementia and other neurological and neurodegenerative disorders. Football players with high scores on depression tests were also found to have higher levels of concussions.
Treatment

Symptoms normally go away without medication in a mild case of TBI. Repeated, mild TBIs, however, can be dangerous or fatal. That is why rest and prevent further exposure are necessary before a doctor gives the go-ahead.
More serious cases, likely with intensive care, would require hospitalisation.
Emergency care is intended to improve the state of the patient and to avoid the aggravation of brain injury.
This will involve ensuring that the airway is open, providing oxygen and ventilation and maintaining blood pressure.
Medications may be used to help control symptoms.
- Sedation: This can help prevent agitation and excess muscle activity and contribute to pain relief. Examples include profanol.
- Pain relief: Opioids may be used.
- Diuretics: These increase urine output and reduce the amount of fluid in tissue. These are administered intravenously. Mannitol is the most commonly used diuretic for TBI patients.
- Anti-seizure medication: A person who has experienced moderate to severe TBI may have seizures for up to a week after the incident. Medication may help prevent further brain damage that may result from a seizure.
- Coma-inducing medications: During a coma, a person needs less oxygen. Sometimes, a coma may be deliberately induced coma if the blood vessels are unable to supply adequate amounts of food and oxygen to the brain.
Surgery
Surgery may be necessary in some cases.
- Removing a hematoma: Internal bleeding can cause partly or fully clotted blood to pool in some part of the brain, worsening the pressure on the brain tissue. Emergency surgery can remove a hematoma from between the skull and the brain, reducing pressure inside the skull and preventing further brain damage.
- Repairing a skull fracture: Any part of the skull that is fractured and pressing into the brain will need to be surgically repaired. Skull fractures that are not pressing into the brain normally heal on their own. The main concern with a skull fracture is that forces strong enough to cause it may have caused further, underlying damage.
- Creating an opening in the skull: This can relieve the pressure inside the skull if other interventions have not worked.
Long-term treatment
Medications may be used to help control symptoms.
- Sedation: This can help prevent agitation and excess muscle activity and contribute to pain relief. Examples include profanol.
- Pain relief: Opioids may be used.
- Diuretics: These increase urine output and reduce the amount of fluid in tissue. These are administered intravenously. Mannitol is the most commonly used diuretic for TBI patients.
- Anti-seizure medication: A person who has experienced moderate to severe TBI may have seizures for up to a week after the incident. Medication may help prevent further brain damage that may result from a seizure.
- Coma-inducing medications: During a coma, a person needs less oxygen. Sometimes, a coma may be deliberately induced coma if the blood vessels are unable to supply adequate amounts of food and oxygen to the brain.
Surgery
Surgery may be necessary in some cases.
- Removing a hematoma: Internal bleeding can cause partly or fully clotted blood to pool in some part of the brain, worsening the pressure on the brain tissue. Emergency surgery can remove a hematoma from between the skull and the brain, reducing pressure inside the skull and preventing further brain damage.
- Repairing a skull fracture: Any part of the skull that is fractured and pressing into the brain will need to be surgically repaired. Skull fractures that are not pressing into the brain normally heal on their own. The main concern with a skull fracture is that forces strong enough to cause it may have caused further, underlying damage.
- Creating an opening in the skull: This can relieve the pressure inside the skull if other interventions have not worked.
Long-term treatment
An individual experiencing severe TBI may need rehabilitation.
They will need to relearn how to walk, speak and perform certain daily activities, depending on the degree and severity of their injury.
It could include hospital or advanced rehabilitation center care. Depending on the type of injury it can include a physical therapist, an occupational therapist and others.
Tips for recovery
Tips that can aid recovery:
- Avoid activities that could cause another blow or jolt to the head.
- Follow the instructions of healthcare professionals.
- Do not take drugs that the physician has not approved.
- Do not return to normal activities, including driving and sports participation, until the doctor agrees.
- Get plenty of rest.
Following the orders of the doctor after a TBI is crucial, because the effect of a brain injury can be serious, and it is not always immediately apparent.
Types
There are two major types of TBI: open and closed. In open TBI, the skull is broken. In a close TBI, it is not.
Further classifications include:
Concussion: A shock of direct effect which may or may not cause a loss of consciousness. This is the most prevalent form of TBI. Often it’s mild but it can be fatal.
Contusion: If a direct hit triggers localized bleeding in the brain, this may lead to a blood clot.
Diffuse axonal injury: When tears occur in the structure of the brain due to skull shearing.
Penetrating injury: When the brain hits a sharp surface.
Causes

TBI is caused by a severe jolt or head blow, or a head injury that penetrates and interferes with normal brain function.
The human brain is protected by the cerebrospinal fluid around it, against jolts and bumps. Within the skull the brain floats in this fluid.
A violent blow or jolt to the head can push the brain against the skull’s inner wall which can cause fibers to tear and bleed within and around the brain.
According to the CDC in 2013 TBI’s leading causes in the U.S. were:
- Falls: Responsible for 47 percent of reported cases, notably in children aged up to 14 years and adults aged over 65 years
- Motor vehicle accidents: These accounted for 14 percent of cases, especially in the 15 to 19-year age group.
- Being struck by or colliding with an object: 15 percent of TBIs resulted from a collision with either a moving or stationery object.
Other causes include domestic violence and work-related and industrial accidents.
Complications
A TBI may have long-term effects and complications, in addition to the immediate risks.
Seizures: These can occur during the first week following the injury. TBIs do not tend to raise the risk of developing epilepsy, unless significant traumatic brain injuries have occurred.
Infections: Meningitis can occur when the meninges, the membranes around the brain, have a rupture. A breaking can allow bacteria to get in. If the infection spreads to the nervous system, it could result in serious complications.
Nerve damage: If the base of the skull is affected, this can affect the face’s nerves, causing facial muscle paralysis, double vision, eye movement problems and a loss of smell sensation.
Cognitive issues: Individuals with moderate to severe TBI may experience some cognitive problems including:
- focus, reason, and process information
- communicate verbally and nonverbally
- judge situations
- multitask
- remember things in the short term
- solve problems
- organize their thoughts and ideas
Changes in personality: These could occur during recovery and rehabilitation. Impulse control of the patient may be altered, resulting in improper behaviour. Changes in personality can cause stress and anxiety on the part of family members , friends and carers.
Problems with the senses: These may lead to:
- tinnitus, or ringing in the ears
- difficulty recognizing objects
- clumsiness, due to poor hand-eye coordination
- double vision and blind spots
- sensing bad smells or a bitter taste
Staying in a comatose state will finally awaken and resume normal life for a long time, but some people may wake up with long-term complications and disabilities. Some people absolutely do not wake up.
Long-term neurological problems: An increasing body of research has linked TBI to depression, Alzheimer’s disease, Parkinson’s disease, and other cognitive and neurological disorders.
Diagnosis
A serious TBI constitutes a medical emergency. Rapid diagnosis and treatment can prevent complications which could potentially threaten life.
The Glasgow Coma Scale
The Glasgow Coma Scale (GCS) is commonly used after a head injury to assess the likelihood and severity of brain damage.
Scores are given according to verbal responses, physical responses and how easily the person can open his or her eyes.
Eyes:
- do not open
- open in response to pain
- open in response to voice
- open spontaneously
Verbal response:
- makes no response
- makes incomprehensible sounds
- utters words or phrases
- speaks but is confused and disoriented
- communicates normally
Motor or physical response
- makes no movement
- extends arm in response to pain
- flexes arm in response to pain
- moves away in response to pain
- can pinpoint where the pain is
- obeys commands to move a part of the body
The score will be added together, and brain injury will be classified as follows:
- Coma, if the score is 8 or less
- Moderate, if the score is from 9 to 12
- Minor, if the score is 13 or more
People who score on the scale of 13 to 15 when they enter the hospital are normally expected to get a good result.
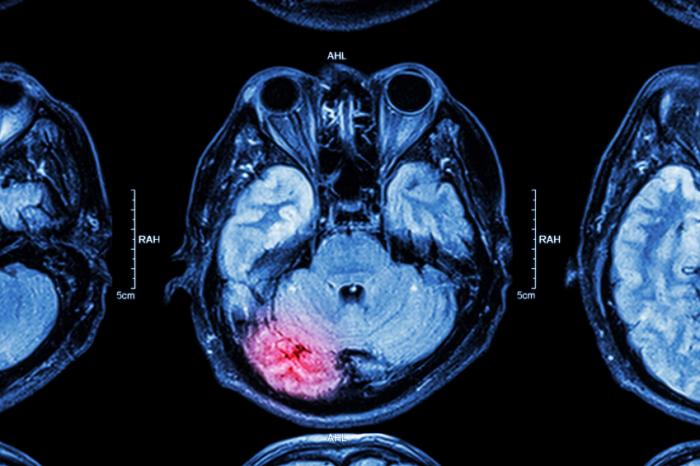
Image scans
MRI or CT brain imaging scans can help decide whether any brain injury or damage has occurred and when.

Angiography can be used to diagnose any blood vessel complications, for example, after a penetrating head trauma.
Electroencephalography ( EEG) measures the electrical activity inside the brain. The findings will indicate whether a patient is having non-convulsive seizures.
Intracranial pressure control allows the doctor to assess the pressure inside the skull. This can show some inflammation in brain tissue.
Neurocognitive assessments can help determine any lack of memory or ability to interpret thoughts.
Patients or caregivers should ensure that health providers know of any medications the person normally takes, especially blood thinners, such as warfarin ( Coumadin), as these can increase the risk of complications.
Prevention
Some tips can reduce the risk of a TBI.

- Always use a seat belt when driving or traveling in a car
- Children should use a suitable restraint for their age and size
- Never drive after drinking alcohol
- Use a helmet when playing sports or using a vehicle where an incident could involve a head injury
- Instal grab bars in a bathroom that is used by older people
- Use nonslip mats on floors that can get wet
- Remove trip hazards, such as loose carpets and trailing wires
- Install window guards and safety gates on stairs if there are children around
- Ensure that play areas are made of a shock-absorbing surface, such as wood mulch
- Store any firearms, unloaded, in a locked safe or cabinet, and keep the bullets in a different location
Extra caution should be taken while supervising young children or older adults. Household adaptations, such as ramps and window guards, may be required.
The American Academy of Family Physicians advises that everyone will go to a hospital after a hit to the head. If someone else hits their head and is behaving in an unusual way, the person who sees it will contact a doctor.
The Heads Up project offers advice and training on how to prevent or deal with a TBI and its effects.