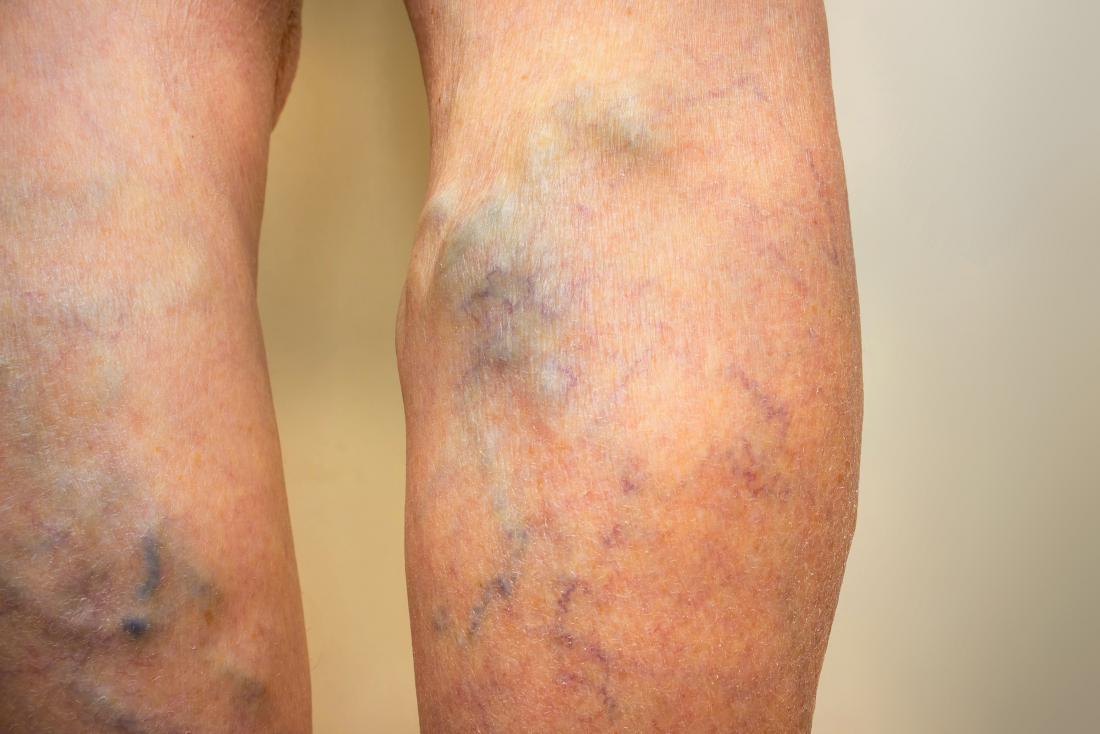
Tiny, damaged veins that may appear on the surface of the legs or face are spider veins. Typically, they are not painful or harmful, but for cosmetic purposes, some people may wish to treat them.
Spider veins can appear in the form of thin lines, webs, or branches and can be blue, purple, or red. People refer to them as thread veins often, too.
Spider veins may be eliminated or their presence minimized by a variety of therapies.
We address the causes of spider veins in this article and how they vary from varicose veins. We also address the treatment and prevention of spider veins.
Causes
Spider veins can occur in the legs when the valves inside the veins stop working correctly.
Blood is transported back to the heart by veins. They have a one-way valve to prevent blood from flowing backwards, which closes after the blood passes through it.
The blood can struggle to flow in the correct direction if this valve weakens or becomes impaired, and it may begin to pool inside the vein. This can cause a bulge in the vein over time that branches out, resulting in spider veins.
Spider veins on the face are often the result of tiny blood vessels bursting. This can happen as a result of increased pressure or sun damage.
Spider veins and varicose veins
Different types of a medical disorder called venous insufficiency are spider veins and varicose veins. In the legs, these conditions are the result of valves in the veins being compromised or impaired. The two problems, however, have distinct symptoms.
Small, thin lines that may be flat or just slightly elevated are typically spider veins. Sometimes, they are blue, red or purple. While they can cause some discomfort, most of the time, they are painless.
Varicose veins are larger and deeper than spider veins. Lumpy or twisted, they may also appear and are usually flesh-colored or red.
Varicose veins can cause a variety of symptoms according to their severity. This may include:
- pain
- itching
- bleeding
- swelling of the legs or ankles
- an achy or heavy feeling in the legs
Varicose veins can also increase the risk of blood clots and problems with circulation in an individual.
Risk factors
Factors that can raise the risk of a person developing spider veins include:
- Genetics: Up to 90% of people with spider veins have a history of getting them in the family.
- Pregnancy: In addition to the extra weight of the fetus, increased blood passing through the body brings more strain on the veins of the leg during pregnancy. Some females report that after pregnancy, spider veins vanish, but they may be permanent.
- Being female: Spider veins appear to be more likely to affect women than men.
- Being older: With time, the valves in the veins begin to get weaker. As an individual ages, the calf muscles, which help support the veins in the legs and allow them to pump blood upwards, may also lose some of their strength.
- Being overweight: Extra body weight will put additional pressure on the veins of the leg.
- Hormones: Hormonal birth control and menopause hormone therapy can increase the risk of spider veins because vein valves can be damaged by estrogen.
- Sitting or standing for long periods: when a person stays in the same place for several hours at a time, veins in the legs have to work harder to pump blood up to the heart.
- A prior blood clot or damage to the vein: This can harm the valves and render them unable to operate properly.
- Excess pressure in the face: This can be caused by coughing, sneezing, or vomiting with force. After pushing during childbirth, some women can get spider veins on their faces.
- Sun damage: Ultraviolet sunlight can damage the skin and, especially on the face, cause broken blood vessels or spider veins.
Treatment
While usually harmless, spider veins may cause discomfort and, for cosmetic reasons, some people may want to treat or remove them.
There are several distinct treatment options available:
Compression stockings or socks

In the lower legs, wearing compression stockings or socks puts pressure on the veins. This pressure will help to increase the flow of blood and avoid more varicose veins or spider veins. Compression stockings can also help to alleviate the swelling of the legs and minimize the risk of leg blood clots.
Compression stocking types include:
- Support pantyhose: These provide only light pressure, but in many stores they are available.
- Stockings and socks with gradient compression: These provide medium pressure across the feet, ankles, and calves. Also they are accessible from specialty shops and pharmacies.
- Prescription compression stockings: These provide the feet and legs with the most strain. They are only available by prescription and come in different sizes and strengths as well as variants that are footless. For certain individuals, including those who have heart failure or other heart conditions, prescription compression stockings are not appropriate.
Sclerotherapy and closure system
Sclerotherapy requires directly injecting an irritant into the vein affected. They stick together to prevent blood from flowing into the region when the walls of the vein become irritated.
This procedure will decrease swelling and cause shrinkage of the vein. The spider vein fades or vanishes over time. To achieve the desired results, several treatments may be required.
Closure system treatment, similar to sclerotherapy, includes injecting a substance into the damaged veins. This material is sticky and closes off the blood supply from the vein, causing the spider vein to fade or vanish over time.
As with sclerotherapy, until they are satisfied with the result, a person can need several treatments.
Professionals in healthcare who can conduct sclerotherapy or method of closure include:
- dermatologists
- vein specialists
- plastic surgeons
- cosmetic surgeons
- trained nurses
Sclerotherapy or closure system may be done in their office by these practitioners as the treatment typically does not require anesthesia.
The person normally wears compression stockings for several days or weeks after undergoing sclerotherapy or closure system. After these treatments, spider veins will gradually begin to disappear, but the process can take up to 6 weeks.
To get rid of spider veins, some individuals need several treatments.
Laser treatment
A laser can be used by a healthcare professional to treat spider veins that are less than 3 millimeters very near to the skin’s surface. The laser is a strong, concentrated light beam that causes the spider vein to clot and dry up.
Since there is no injection, laser therapies are less painful than sclerotherapy or closure systems.
Laser Endovenous Therapy (EVLT)
For the treatment of spider veins and small varicose veins, EVLT is a newer method.
A healthcare professional makes a small incision and then implants a laser fiber into the affected vein. The laser directly adds heat to the vein and causes it to collapse. It can take several months or up to a year for the vein to vanish.
EVLT involves the use of local anesthesia.
Surgery
Although certain surgical treatments for larger varicose veins may be successful, doctors do not generally perform them on spider veins. The explanation for this is that spider veins are small, so the less invasive treatments above often respond well to them.
Prevention

Some lifestyle improvements and self-care tips can help avoid the emergence of new spider veins or stop the deterioration of existing ones. They include:
- Sunscreen wearing. Every day, applying sunscreen can help prevent some spider veins, particularly on the face. When outside for long periods, use sun-protective hats and clothes.
- The maintenance of a healthy weight. It helps to decrease pressure on the veins and keeps blood circulating well.
- Wearing compression stockings. Consider using compression stockings or socks if spider veins or varicose veins are a problem or run in the family.
- Staying mobile. Avoid sitting or standing without taking a break for long periods. Get up every 30 minutes and walk around.
- The avoidance of tight clothes. Over-tight clothing around the waist, legs, or pelvis can reduce the flow of blood and increase the risk of spider veins.
- Avoiding the overuse of saunas and hot tubs. Excessive heat may cause veins to swell, raising the risk of veins in the legs being dilated and bulging.
- Limiting alcohol consumption. In some individuals, drinking alcohol can trigger flushing in the face and broken blood vessels.
- Having to workout daily. Physical exercise can help to increase circulation and avoid the pooling of blood in the legs.
- Uplifting legs. When sitting or lying down, raising the legs will help prevent blood from pooling downwards in the legs.
- To see a dermatologist. In order to explore treatment options, people with skin disorders that may raise the risk of spider veins, such as rosacea, may want to consider seeing a doctor or dermatologist.
- Using cover-up products. If the presence of spider veins is a problem, individuals may also use body or leg makeup to temporarily cover or eliminate them. For this reason, self-tanning products can also work.
Conclusion
The result of damaged veins or burst blood vessels is spider veins. Usually, they are painless and may not cause health complications, although for aesthetic purposes, certain people may wish to treat them.
A variety of treatment methods can help enhance or fully eliminate the presence of spider veins. Consulting a licensed healthcare practitioner who specializes in dermatology, vein treatment, or cosmetic or plastic surgery is often necessary for medical procedures.