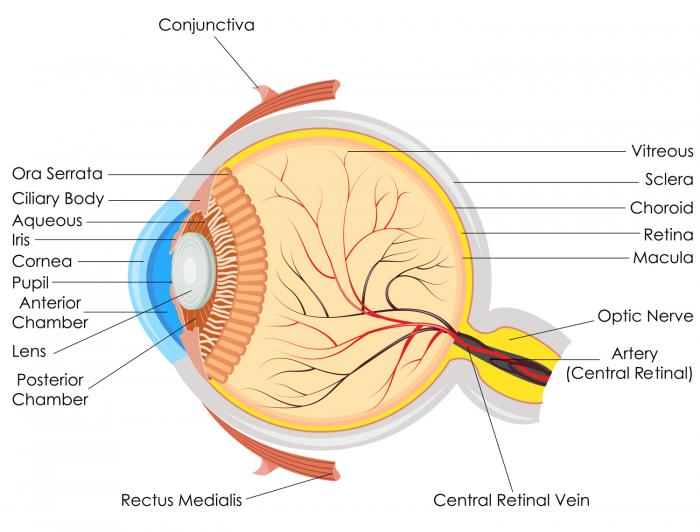
Macular degeneration is a disease that affects the retina, the rear layer of the eyeball. This layer contains light-sensitive cells. It aids our perception of the world around us.
The central vision is affected by age-related macular degeneration (AMD). Images that were previously clear may become hazy, and black patches may emerge, growing bigger.
Colors are darker or less vibrant than they used to be, and straight lines may look twisted or warped.
Reading, writing, recognizing people, and driving are all becoming more difficult. However, peripheral vision is normally enough to allow for other everyday tasks. It’s improbable that you’ll lose all of your sight.
It primarily affects older people and is a leading cause of partial blindness in people aged 50 and over.
What is AMD, and how does it work?
Macular degeneration is explained in the video below, as well as how it impacts vision.
Causes

Although the specific cause of AMD is unknown, a variety of risk factors have been identified. Excess weight, high blood pressure, smoking, and a family history of the condition are all risk factors.
Types
Wet and dry macular degeneration are the two types of macular degeneration.
- Dry macular degeneration is a kind of macular degeneration that occurs over time. There is no therapy available. There are coping mechanisms that the sufferer can acquire. In 85 to 90 percent of situations, the dry form is used.
- Wet macular degeneration, sometimes referred to as neovascular AMD, occurs when new blood vessels form underneath the macula. These can lead to the loss of blood and fluid. Wet AMD is a more dangerous form of AMD that can cause significant visual loss. It has the potential to evolve more swiftly. If symptoms arise, they must be treated right away.
Risk factors
According to statistics from 2010, AMD impacted 2.1 percent of people over the age of 40 in the United States. This rate was 2.5 percent among white people, increasing to almost 14 percent for those over 80 years old. Figures for other ethnic groups are lower.
Macular degeneration can affect younger people in rare situations. Stargardt’s disease (STGD) and Best’s disease are examples of juvenile macular degeneration. It is mainly caused by a hereditary condition.
Key variables that appear to play a role, according to the American Academy of Ophthalmology (AAO), include:
Age: After the age of 60, the danger becomes higher.
Ethnicity: AMD is more common in Caucasians than in other ethnic groups.
Family background: Around 15 to 20% of people with AMD have a close family who suffers from the condition.
Cigarette smoking: Current smokers are four times as likely than nonsmokers to get AMD.
Obesity: Excess weight or obesity, in combination with other risk factors including high blood pressure and cholesterol, appears to increase the risk.
There are various risk factors in both AMD and cardiovascular disease (CVD). Lifestyle actions that lower the risk of CVD, such as quitting smoking and decreasing dietary fat consumption, may also lower the risk of AMD.
Other things to consider are:
- Exposure to light: Some studies suggest that high-energy visible light and ultraviolet (UV) light, such as sun exposure, may have a role, but others disagree. There was no correlation, according to a study published in JAMA Ophthalmology in 2001. Most eye physicians, however, advise that you wear UV-protective sunglasses.
- Dietary fat: According to studies, people who consume a lot of saturated fats are more likely to get AMD.
Symptoms
AMD causes subtle alterations in the body. Most people aren’t aware they have it until it’s too late, when vision loss begins.
Blurring of the person’s center vision is the most common symptom. Outer vision (peripheral vision) is unaffected. Even when the person wears glasses, the blurred central vision persists.
Dry AMD symptoms:
Dry AMD symptoms might take up to ten years to show, and even longer if the disease only affects one eye.
If symptoms do occur, they may include the following:
- colors seeming less vibrant than they used to
- increasing difficulty recognizing people’s faces
- hazier, less defined vision
- the need for a brighter light when reading
- written or printed texts appearing blurry
- slow recovery of visual function after exposure to bright light
Wet AMD symptoms:
All of the aforementioned symptoms, as well as the following, may be present:
- metamorphopsia, in which straight lines appear crooked or wavy
- a blind spot in the central vision (central scotoma) that will get bigger without treatment
When compared to dry AMD, symptoms develop and worsen more quickly.
Early AMD does not usually develop to the later stages, according to the National Eye Institute (NEI).
- After ten years, around 1 in 20 people with early AMD in one eye and normal eye in the other will develop advanced AMD.
- After ten years, around 14% of people with early AMD in both eyes will have late AMD in one or both eyes.
Early AMD can be detected with regular eye examinations, and actions can be done to limit the chance of it worsening.
Diagnosis

It is important to contact an eye doctor, optometrist, or ophthalmologist if vision difficulties develop.
The eyes, particularly the rear of the eyes, where the retina and macula are located, will be examined by the eye expert.
Following that, a number of tests will be conducted:
Amsler grid: The patient examines a unique grid made up of vertical and horizontal lines. Some of the lines on the grid may seem distorted, broken, or faded if AMD is present.
The outcome will provide a better indication of the extent of the harm. The lines closest to the center of the grid seem distorted, faded, or broken to most people with discernible symptoms.
Fluorescein angiography: This test determines the type of AMD you have. When a specialist detects wet AMD, this procedure is frequently performed.
The doctor will inject a special dye into the patient’s arm and then use a special magnification instrument to examine their eyes. They’ll photograph the eye in succession. If the blood vessels behind the macula are leaking, the images will show it.
When blood vessels leak below the macula, wet AMD develops.
Optical coherence tomography: The retina is scanned and an image is taken using special light rays. The scan provides the professional with further information regarding the macula. The scan may tell if the macula has thickened, thinned, or altered in any manner.
Treatment
It is advised to have regular eye exams to detect macular degeneration before vision loss occurs.
Treatment will not be able to restore eyesight, but it will help to halt the progression of visual loss.
Dry AMD
Dry AMD rarely causes total vision loss, and peripheral vision is frequently preserved.
Support and lifestyle changes can make it easier to live with vision loss and optimize the vision is left.
The following are some suggestions:
- using intensive reading lights
- getting large print books
- using a magnifying lens
Wet AMD
Some therapies can stop the growth of wet AMD, also known as neovascular AMD, but they must be administered quickly to be successful. Any loss of vision is extremely difficult to restore.
Anti-VEGF medication
Anti-vascular endothelial growth factor medicine (VEGF) is a drug that helps people with wet AMD create new blood vessels in their eyes. Anti-VEGF medications inhibit the production of new blood vessels by blocking this molecule.
Ranibizumab (Lucentis) and bevacizumab are two examples of these medications (Avastin).
After administering anesthetic, the doctor uses a very thin needle to inject the medication into the eye.
Every few weeks, the therapy must be repeated.
Anti-VEGF therapy has helped some people regain their eyesight, but it all depends on the individual and their symptoms.
Anti-VEGF therapy normally has no adverse effects, although the injections might cause pain, swelling, redness, and impaired vision.
Treatment can result in problems such as injury to the retina, damage to the lens of the eye, and infection in extremely rare circumstances.
Photodynamic therapy
A light-sensitive drug called verteporfin is injected into the person’s arm. Veteporfin binds to the proteins found in the veins. In the macula, it can identify aberrant blood vessels.
For roughly a minute, a laser is flashed through the eye. The aberrant blood vessels in the macula are eliminated when verteporfin is stimulated by the laser. This occurs without causing any harm to the eye’s surrounding tissue. Blood or fluid cannot seep out and further harm the macula if the vessels are damaged.
Every few months, some individuals require photodynamic treatment. Whether or not this sort of therapy is used is determined on the location of the target blood vessels and how profoundly they have impacted the macula.
This is a less prevalent therapy than anti-VEGF injections.
Laser therapy
A laser may be used by an eye specialist to treat aberrant blood vessels in the retina. This is likewise not used as frequently as other treatments, although in some circumstances it may be beneficial.
Home remedies
Some supplements, according to research, may help slow the growth of AMD.
Antioxidants, vitamins, and minerals
The following components have been demonstrated to be beneficial in studies when given during the intermediate or later stages:
- copper oxide (cupric oxide 2 mg)
- lutein (10 mg)
- zeaxanthin (2 mg)
- vitamin C (500 mg)
- vitamin E (400 IU)
- zinc oxide (80 mg)
The supplements, known as Age-Related Eye Disease Studies (AREDS and AREDS2) supplements, are available without a prescription, but patients should consult a doctor first to confirm they are getting the right kind.
Vitamins aren’t a cure for AMD, but they can help slow down the growth of the disease.
Omega-3 fatty acids
In 2008, a meta-analysis indicated that a high dietary consumption of omega-3 fatty acids, which are present in flax and fish oils, was connected to decreased levels of AMD. The data, however, was not strong enough to warrant the use of omega-3 supplements to prevent the disease, according to the researchers.
In 2015, another study revealed that there was no relationship between the two.
Stem-cell therapy
Human stem cells may one day enable the retina to mend itself, according to research.
The BMJ reported in March 2018 that two people with very severe wet AMD had their sight restored following stem-cell treatment.
Implantable telescope
Another study indicated that an implanted micro telescope (IMT) might help people with advanced AMD see better. The return of some vision and a higher degree of independence are among the advantages. However, the person’s range of vision will be limited, and he or she will still be unable to drive.
Complications
AMD can cause a variety of problems.
Adapting to the loss of vision: It’s difficult to accept vision loss, especially when formerly simple things like reading become challenging. Stress, sadness, and anxiety might result as a result of this. Speaking with a health expert may assist a person in discovering new coping mechanisms.
Driving: A person’s ability to drive can be harmed by AMD. If a person’s visual changes may influence their ability to drive, an eye doctor can counsel them.
Risk of cardiovascular disease: AMD and CVD share several risk factors, and studies show that people with AMD are more prone to develop CVD symptoms.
Visual hallucinations: Some people may be affected if their vision deteriorates significantly. This might be because the brain creates imagination representations, frequently from memory, to compensate for missing visual input.
Some individuals are hesitant to discuss this because they are concerned that it might signal a mental condition. It’s important to understand that these hallucinations are caused by eye issues, not a change in mental state.
Sources:
- https://nei.nih.gov/eyedata/amd
- https://ghr.nlm.nih.gov/condition/age-related-macular-degeneration
- https://www.ncbi.nlm.nih.gov/pubmed/18541848
- https://jamanetwork.com/journals/jamaophthalmology/fullarticle/268111
- https://nei.nih.gov/health/maculardegen/armd_facts
- https://www.ncbi.nlm.nih.gov/pubmed/18345009
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4909674/
- https://www.ncbi.nlm.nih.gov/pubmed/25856365
- https://www.medicalnewstoday.com/articles/152105
- https://medlineplus.gov/maculardegeneration.html
- https://www.bmj.com/content/360/bmj.k1290.full
- https://jamanetwork.com/journals/jamaophthalmology/fullarticle/267470
- https://www.aao.org/eye-health/news/top-5-risk-factors-amd
- https://www.aoa.org/patients-and-public/caring-for-your-vision/uv-protection
- http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0089600