A pulmonary embolism is a pulmonary artery blockage that provides the blood to the lungs. It is one of the most prevalent cardiovascular diseases in the USA.
Every year about 1 in 1,000 people in the US are affected by pulmonary embolism.
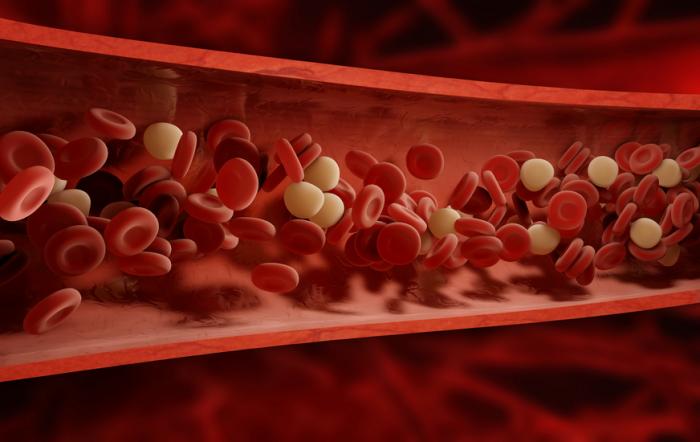
The blockage, which is normally a blood clot, prevents oxygen from entering lung tissues. This means it can endanger life.
The word “embolism” derives from the Embolos in Greece, meaning “stopper” or “plug.”
The embolus arises in one region of the body in a pulmonary embolism, it circulates in the blood stream, and then prevents the blood flowing through a channel to another region of the body , including the lungs.
An embolus is distinct from a thrombus that develops and stays in one position.
Symptoms

Symptoms of pulmonary embolism include:
- chest pain, a sharp, stabbing pain that might become worse when breathing in
- increased or irregular heartbeat
- dizziness
- difficulty catching breath, which may develop either suddenly or over time
- rapid breathing
- a cough, normally dry but possibly with blood, or blood and mucus
Severe signs call for urgent medical assistance.
More serious cases may lead to shock, loss of consciousness, cardiac arrest and death.
Treatment

Treatments for embolism aim to:
- stop the clot from growing
- prevent new clots from forming
- destroy or remove any existing clot
Treating shock and providing oxygen therapy is a first step in treating most embolisms.
Anticoagulant medications, such as heparin, enoxaparin, or warfarin are typically administered to help thin the blood and avoid further coagulation.
Individuals who require anticoagulant medications should seek treatment with an anticoagulant control program, not their primary care doctor.
These can also be applied to clot-busting medications called thrombolytics. Yet such bear a high chance of heavy bleeding. Activase, Retavase, and Eminase include thrombolytics.
When the patient has low blood pressure, he may be given dopamine to raise the pressure.
The patient would typically be expected to take medicine continuously for an unspecified period of time , usually for at least three months.
Prevention
A number of measures can reduce the risk of a pulmonary embolism.
- A high-risk patient may use anticoagulant drugs such as heparin or warfarin.
- Compression of the legs is possible, using anti-embolism compression stockings or pneumatic compression. An inflatable sleeve, glove, or boot holds the affected area and increases pressure when required.
Methods of compression prevent blood clots by forcing the blood into deep veins and reducing pooled blood.
Many ways of lowering the risk include physical activity, daily exercise, a balanced diet and giving up or preventing cigarette use.
Causes

A pulmonary embolism occurs when the blood flowing into an artery supplying the lungs becomes blocked by an embolus, usually a blood clot.
A blood clot, known as deep venous thrombosis (DVT), can begin in an arm or leg.
It breaks free after that, and travels towards the lungs through the circulatory system. There, passing through the small vessels is too large so it forms a blockage.
This blockage stops the flow of blood into a part of the lung. This causes the lung section that has been affected to die from lack of oxygen.
Rarely may a pulmonary embolism result from an embolus created by fat droplets, amniotic fluid, or some other substance that flows into the bloodstream.
Diagnosis
To reach a diagnosis, the doctor will look at the patient’s history and consider whether an embolism is likely. They will carry out a physical examination. Diagnosis can be challenging because other conditions have similar symptoms.
Tests for diagnosing pulmonary embolism include:
- a mathematical model that helps a doctor predict the course of DVT and the risk of an embolism
- d-Dimer test, a blood test that can diagnose thrombosis that can rule out further testing if it produces a negative result
- pulmonary V/Q scan, two tests that analyze the ventilation and structural properties of the lungs and give off less radiation than a CT
- computerized tomography (CT) scan, which can reveal abnormalities in the chest, brain, and other organs, and in cases where a V/Q is not possible
- electrocardiogram (EKG), to record the electrical activity of the heart
- arterial blood gas study, to measure oxygen, carbon dioxide, and other gases in the blood
- chest X-rays, to generate a picture of the heart, lungs, and other internal organs
- ultrasound of the legs, to measure the speed of blood flow velocity and any changes
- pulmonary angiogram, to reveal blood clots in the lungs
- magnetic resonance imaging (MRI), to obtain detailed pictures of internal structures
Risk factors
With age the risk of developing a pulmonary embolism increases. Individuals with disorders or diseases that increase blood clotting risk are more likely to experience pulmonary embolisms.
An individual has a higher risk of pulmonary embolism if he or she has had a blood clot in his or her leg or arm (DVT) or has had a pulmonary embolism in the past.
Long periods of bed rest or inactivity raise the risk of DVT and hence the risk of pulmonary embolism increases. This might be a long flight or a ride by car.
Our blood collects in the lower parts of our body, when we don’t move much. If blood travels faster than average it is more likely to form a blood clot.
Damaged blood vessels also contribute to the risk. That may happen due to injury or surgery. If a blood vessel gets damaged, the inside of the blood vessel may get narrower, increasing the chances of forming a blood clot.
Certain risk factors include some cancers, inflammatory bowel disease, obesity, pacemakers, vein catheters, pregnancy, supplements of oestrogen, a family history of blood clots, and smoking.
Outlook
Most people who suffer a pulmonary embolism will make a complete recovery with successful and timely treatment.
The disease carries an increased risk of death. Early treatment, however, can dramatically reduce that risk.
Highest risk period is in these hours after the embolism occurs first. The situation often gets worse when an underlying illness, such as a form of cancer, caused the embolism.
Most people with pulmonary embolism will do a complete recovery, however.